Surrogate Endpoints for Neuroscience Clinical Trials: Challenges & Progress
Surrogate endpoints as the basis for neuroscience clinical trials, amyloid and Alzheimer's disease, and the future role of biomarkers for CNS
In neuroscience drug development, surrogate endpoints hold the promise of expediting clinical trials and bringing therapies to patients faster. These endpoints serve as proxy markers that predict clinical benefit without requiring direct evidence of improved patient outcomes. However, while surrogate endpoints have transformed the treatment of cancer, their application in neuroscience has been fraught with challenges. This post explores the current landscape of surrogate endpoints in neuroscience, the hurdles unique to this domain, a case study on Alzheimer’s disease, and thoughts on innovation in the field.
What Surrogate Endpoints Exist for Neuroscience Indications?
The FDA currently lists a table of >100 surrogate endpoints that have been “the basis of approval or licensure (as applicable) of a drug or a biological product.” While many cancers and rare diseases are included, only three surrogate endpoints have been used in conditions that fall into neuropsychiatric indications.
Alzheimer’s Disease:
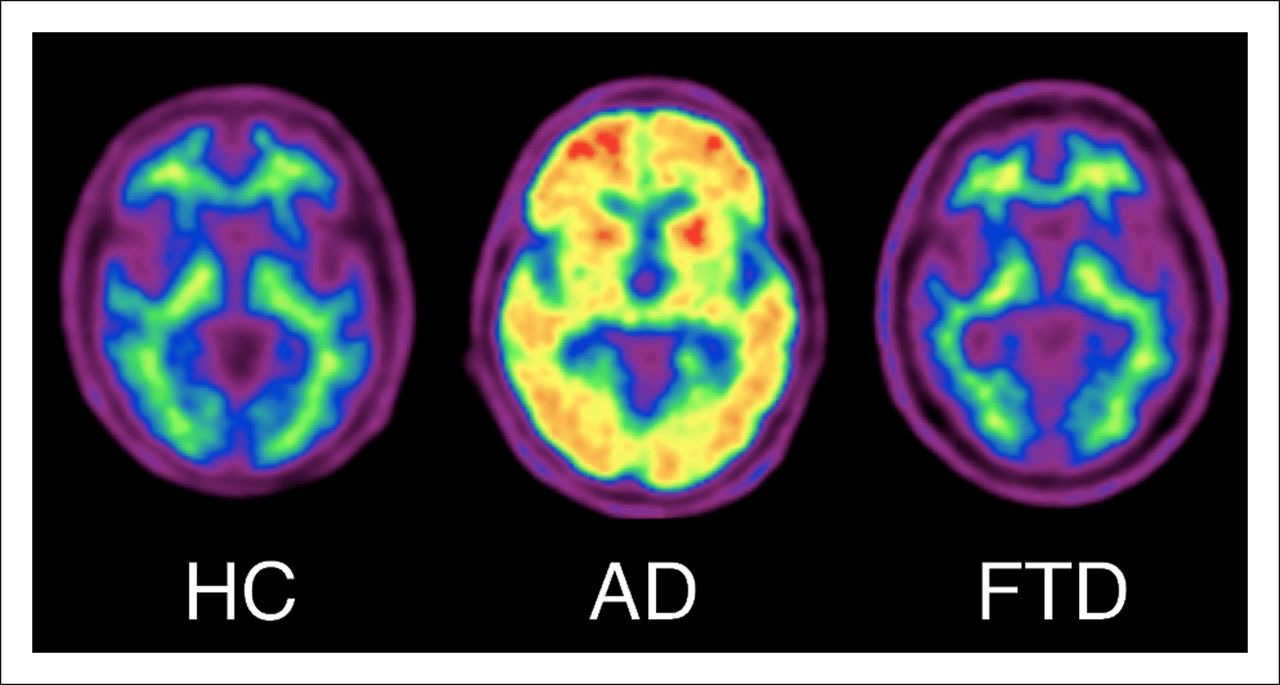
Reduction in amyloid beta plaques, as measured by amyloid PET imaging, is a widely used surrogate endpoint. The accelerated approval of aducanumab (Aduhelm) by the FDA in 2021 hinged on this marker, even though its clinical efficacy remains debated.
Since aducanumab’s mechanism of action (and other anti-amyloid therapies like lecanemab (Leqembi)) is through direct reduction of amyloid formation, this strategy significantly increases likelihood of a detectable signal that could be statistically differentiated from placebo.
Substance Use Disorders
Opioid Use Disorder: Urine toxicology tests for opioids can serve as a surrogate for drug abstinence.
Tobacco Dependence: Measurement of exhaled carbon monoxide provides a marker of smoking cessation.
Note again, because opioids and tobacco can be attributed directly to the pathogenesis of the condition (they quite literally define the condition), it is clear why changes in these surrogate endpoints are likely to enhance patient health.
Why Are Surrogate Endpoints So Challenging in Neuroscience?
Developing surrogate endpoints in neuroscience is inherently difficult due to the complexity of brain diseases and the limitations of current measurement tools. For a surrogate endpoint to be viable, it must meet criteria outlined in section 507(e)(9) of the FD&C Act (part of the 21st Century Cures Act), which states that a surrogate endpoint must:
1. Predict clinical benefit to support traditional drug approval.
2. Be reasonably likely to predict clinical benefit for accelerated approval.
Unlike fields like oncology, where single genes or proteins often drive disease processes (and you can easily get a biopsy from patients to measure these molecules), neuroscience is resistant to reductionist approaches. Neurological and psychiatric diseases involve complex, dynamic interactions between molecular, cellular, and network-level changes. This complexity makes it difficult to identify single biomarkers that correlate directly with clinical outcomes.
Moreover, surrogate endpoints (like biomarkers) in neuroscience must be sensitive, specific, responsive, and quantifiable to the treatment being studied. Current technologies, while improving, often fail to meet these stringent criteria. For example, amyloid PET imaging in Alzheimer’s provides a window into disease pathology but doesn’t always align with clinical outcomes like cognitive improvement.
Case Study: Amyloid Load and Aducanumab
The accelerated approval of aducanumab (Aduhelm) for Alzheimer’s disease by the FDA illustrates both the promise and pitfalls of surrogate endpoints. Aducanumab’s approval was based on its ability to reduce amyloid beta plaques, a hallmark of Alzheimer’s pathology. However, the clinical efficacy of aducanumab remains controversial, raising questions about the validity of amyloid load as a surrogate endpoint.

Key Insights from Aducanumab’s Journey:
Amyloid-centric Development from the Start: Biogen’s journey began with amyloid-centric development, which is specific, sensitive, and responsive to their antibody. Biogen’s early Phase 1 trial showed dose-dependent amyloid reduction in the brain and tolerable safety, with the notable occurrence of amyloid-related imaging abnormalities (ARIA). The PRIME Phase 1b study, launched in 2015, demonstrated significant amyloid clearance and exploratory cognitive benefits at higher doses, but also a clear association between ARIA and higher doses, especially in ApoE4 carriers.
Mixed Clinical Benefit in Larger Clinical Trials
Biogen initiated two Phase 3 trials in 2018—ENGAGE and EMERGE—enrolling over 2,700 participants with early Alzheimer’s disease. These trials aimed to assess the clinical efficacy of aducanumab by measuring cognitive and functional decline over 18 months (using the MMSE and CDR-SB). However, a 2019 interim futility analysis predicted failure, prompting Biogen to halt the trials. Later that year, the company controversially revived the program, citing reanalysis showing EMERGE met its primary endpoint, with the highest dose slowing cognitive decline, though ENGAGE missed its endpoint.
FDA Accelerated Approval, EMA Rejection
In 2021, the FDA granted aducanumab accelerated approval based on its ability to clear amyloid plaques, despite ongoing debate over amyloid’s validity as a surrogate endpoint for clinical benefit. The approval sparked intense criticism from scientists and policymakers, highlighting inconsistencies in clinical efficacy between trials and significant safety concerns, including ARIA in one-third of participants. European regulators rejected aducanumab in late 2021, and Medicare severely restricted coverage to patients enrolled in clinical trials. Biogen’s subsequent real-world evidence initiatives and confirmatory Phase 4 ENVISION trial faced challenges, as safety issues and limited efficacy data continued to undermine confidence. In 2023, a U.S. Congressional investigation criticized Biogen and the FDA for their handling of the approval process, leading to Biogen’s announcement in January 2024 to cease marketing the drug and terminate its confirmatory trial.
Advancing the Conversation: The Role of Biomarkers in AD Diagnosis
While Adacanumab’s journey resembles a top tier roller coaster at Six Flags, this marks a very important precedent. The first time a surrogate endpoint was used as the basis of approval in Alzheimer’s disease. This has sparked significant debate (see: “Is Amyloid Load a Valid Surrogate End Point for Alzheimer Disease Clinical Trials?” in JAMA), and begs the need to better define Alzheimer’s. An international working group published their findings on “Alzheimer Disease as a Clinical-Biological Construct” earlier this month. A main finding is that biomarkers should be considered a risk factor, but a clinical diagnosis is necessary. This may be one of the best modern examples of resisting reductionist as a path forward for neuropsychiatric disease diagnosis.
Thoughts on Surrogate Endpoints in Neuroscience
Strive for Precision in Mechanistic Biomarkers: Surrogate endpoints must be tightly linked to the molecular or cellular pathway being targeted. For example, therapies modulating synaptic plasticity could measure markers directly related to this process, such as synaptic density imaging (such as SV2A PET). This proved successful for FDA Approval of aducanumab— an anti-amyloid therapy that needed to demonstrate that amyloid was reduced.
Patient Level Evidence for Biomarkers Should be Extremely Compelling: It is difficult to tell if the surrogate endpoint of amyloid reduction was chosen more for the practical benefit (of being able to perform a statistical test against placebo from a very specific biomarker) than for the convincing ties to clinical progression. Obviously there was an attempt at achieving both of these goals.
While amyloid has been studied extensively, we need to better understand what we believe causality is in neuropsychiatric disease. Modifying biology is near meaningless to society if the trial is successful but patients don’t benefit.
Innovate Beyond Reductionism: Current neuroscience research often relies on reductionist frameworks and statistical correlations. This is the current biomedical model, and it is easy to convince ourselves that if there is a genetic association, that gene product will be causal for disease. Perhaps we need to incorporate mediators or modifiers (e.g. smoking status, age, etc.) into biomarker models to what we assume is causal in assigning a biomarker to disease status. This could be a more refined approach to complex diseases.
Final Musings
Surrogate endpoints represent a critical tool for accelerating neuroscience drug development, but their adoption requires rigorous validation and thoughtful application. The challenges of complexity, measurement limitations, and clinical relevance highlight the need for innovation in this space. By refining biomarkers, creating models with modifiers or mediators on the effects of an association, and balancing reductionist and holistic frameworks, the field can advance toward surrogate endpoints that reliably predict clinical benefit. In doing so, neuroscience can follow in the footsteps of oncology, where surrogate endpoints have transformed the landscape of drug development.
However, the ultimate goal remains unchanged: improving patient outcomes. Surrogate endpoints should serve as stepping stones, not substitutes, for meaningful clinical benefit.


Probably not a 'be all end all', but why not something simple and practical, like a short-term memory test? Perhaps, something that could be administered as on a smart-phone app. The power here could be the development of a baseline and observe the changes longitudinally compared to placebo and even general population.
Maybe this is already being done and I'm behind on the literature.